In the world of modern development of all kinds of legal relationships between people at various levels of interaction and in various fields of activity, medicine is not the last in the need for strict reporting documentation. This is due to the fact that physicians, as a direct link in the functioning of the health-improving and preventive process of any medical institution, assume a certain responsibility for their qualifications and professional actions. In addition, modern doctors are responsible for how their medical prescriptions and recommendations affect the immediate health of patients.
That is why there is a medical file with a lot of personal records, clinical histories of illnesses, discharge reports of patients and other medical documents. Accordingly, even the death of a person is subjected to certain studies and procedures that must be documented in accordance with applicable law governing specifically such cases. This refers to the obligatory conduct of appropriate laboratory manipulations related to the examination of a corpse and postmortem autopsy. The protocol, the design and drafting procedure of which is essential for determining the naturalness or violentness of the death of the deceased, is considered the primary document in forensic forensics.

The essence and purpose of the document
On the example of the protocol of postmortem examination of a person, future medical examiners-criminologists are currently studying at the graduate school. On the basis of this document, the investigating authorities draw appropriate conclusions during the operational search. Extracts from this protocol are appealed by the parties to the proceedings - representatives of the legal profession or the prosecutor's office - at the time of coverage of the evidence or accusation base in the course of a criminal case hearing. In the end, due to the post-mortem diagnostic data extracted from the contents of the protocol, relatives and friends can find out the exact cause of death of the deceased patient. Therefore, the importance and regularity of the need to draw up this document is well founded.
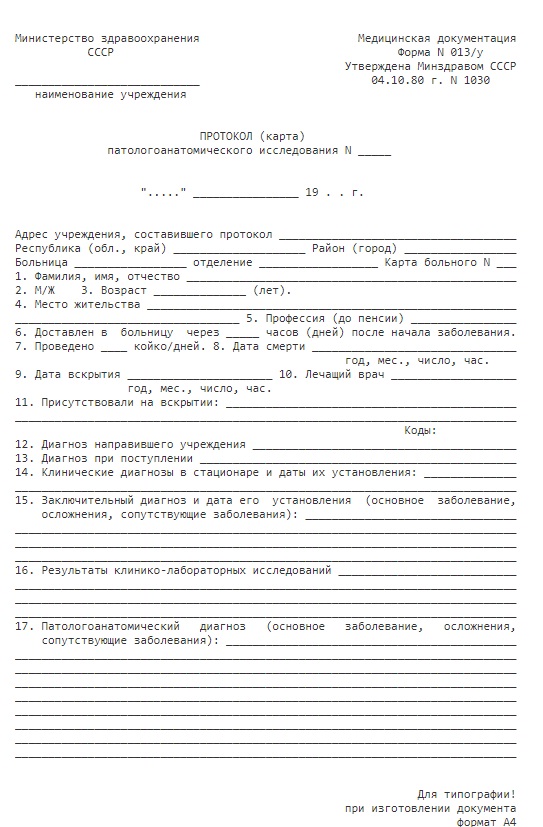
A sample sample of the protocol form can be considered below.
Order of registration
The autopsy protocol of a person according to the model approved by the Ministry of Health is filled in by each individual institution (laboratory, clinic, morgue) performing an autopsy procedure. But until now there is no single universally accepted form of recording post-mortem autopsy and examining the internal organs of a person: some medical departments, departments, institutes and bureaus are guided by order No. 1030 of 1980, which was approved by the USSR, while others use later developments. In any case, the form of the protocol for postmortem examination of a person contains a list of certain elements in the form of sections - there is no significant difference between the forms of various institutions. Only details due to the specifics of the activities of a particular bureau may differ.
In fact, the sample protocol of the pathoanatomical autopsy of a person includes two blocks: the protocol-map of the study itself, which is executed in two copies, and the protocol text itself, which includes a description of the direct examination, microscopic modifications of the organs, and the results of laboratory histological studies. One of the copies of the card along with the text of the protocol is stored in the archive of the pathology department, the other is provided to the head of the medical institution who sent the corpse to an autopsy procedure, along with a medical history, an outpatient card and other medical documents.
The protocol is drawn up under the dictation of the prosector or is recorded immediately after the autopsy. You can also use a voice recorder so that the protocol is subsequently reprinted.

Role in science, medicine, jurisdiction
An autopsy protocol is considered the main document of an expert physician that stores information about the causes of natural or violent death of the deceased. Using the example of the protocol of postmortem examination of an animal, we study the features of documenting the autopsy procedure during in-patient training or conducting workshops for students of veterinary specialization.
The situation is similar with graduate students of forensic medical examination - they also practice with human biological material and learn to correctly record the features identified during the study in the protocol.
Among other things, this kind of medical documentation has legal force, since on the basis of the protocol certain conclusions are made during the consideration of the case by the investigating authorities, people's courts, when clarifying the circumstances or causes of death. Its data should carry the most accurate semantic load and reflect reliable information about the smallest fact revealed during laboratory research. This document should objectively reflect those pathological changes that were discovered during the autopsy and which illuminate the results of the additional examination. After all, it contains certain logical conclusions about the causes of a person’s death, on the basis of which the prosecutor’s office can fully charge, and the bar, in turn, protect the interests of its client, since this examination and its fixation are considered impartial, and the experts who carry it out are not interested.

Information Style
At the time of the description and recording of the information obtained during the study, it is forbidden to use purely medical terminology. The text should be written in plain language for those who are not specialists in the field of medicine and anatomy. First of all, this is done so that the parties and participants in the proceedings can appeal and use the information. So, for example, the description of acute myocardial ischemia, formed due to the splitting or rupture of an atherosclerotic plaque with the subsequent manifestation of a coronary artery thrombus and increased platelet aggregation, is reflected in the documentation simply as myocardial infarction.
The autopsy protocol should clarify and explain the causes of those abnormal phenomena that occurred in the body of the deceased and became a catalyst for his natural or violent death. Similarly, phrases of the type “normal”, “no change” and so on are not allowed to be used, because the description of anatomical changes requires specificity, clarity, accuracy, and brevity. And the document itself should be compiled by a specialist pathologist who directly performed the autopsy, and by persons who were present during the autopsy act. Latin in the writing of the protocol is not allowed.

The first part of the protocol: introduction
Before receiving the autopsy report, the head of the medical institution where the deceased was undergoing therapy, or the investigative and operational committee conducting an investigation to determine the circumstances of the victim's death, sends a request to the appropriate bureau for the forensic medical examination procedure.
The first part of the autopsy report is an introduction. This is the so-called corpse registration. This section provides the following information:
- protocol number in the prescribed manner;
- surname, name, patronymic of the deceased;
- details of his passport;
- gender, age, place of residence;
- Date of death;
- time and place of the examination;
- information about the experts who conducted the examination and were present at the autopsy with the obligatory indication of the position, surname, name, patronymic.
If there is no officially registered civilian information about the deceased, his age is determined by a number of different signs: body weight, volume of forms, tooth position, and so on.
Then, the analytical data that are related to the development of the disease or death of a person are listed, depending on the circumstances under which the person died. First, information about the method and lifestyle is described. If a person was, for example, a drug addict and used the appropriate narcotic drugs, this information is reflected at the initial stage of recording the autopsy procedure. If a medical history has taken place, it should also be indicated in this document. Here, a list of preventive, specific and non-specific measures should be given and the results of allergic and laboratory tests of blood, feces, urine, mucus and other biomaterials that indicate the manifestations of the disease preceding death should be documented. In addition, the introduction of the protocol includes information about the features and symptoms of the disease, treatment measures and medications, the course of treatment and its effectiveness. All this is indicated in the protocol without fail.
After listing information about a person’s disease, information follows about the time and circumstances of death, the clinical diagnosis in the anamnestic data. In addition, the means of transporting the person to the autopsy site is indicated.

Part Two: Descriptive
The second part of the protocol contains a description of the morphological state of organs and tissues both within normal limits and in a state of alteration. Identified during external and internal examination of the corpse, the data of the pathological examination of the corpse are recorded and sequentially presented in the smallest details. This section of the protocol has some fundamental principles of presentation:
- The narrative is compiled without any conclusions and subjective judgments - here, absolutely all the characteristics obtained during the analysis are described accurately, clearly, objectively.
- Recording is conducted in the native language and in accessible simple terms, without the use of Latin or special terminology.
- During external and internal examination of the corpse and organs, methodological methods of the study are described, and the main parameters of the state of the organs of the deceased are correctly and correctly described: their size, shape, location, color of the consistency of the liquid components, the pattern of tissues on the outer surface and in the context of the organ are studied, and odor characteristics, if present, are also described.
- If there are holes and precipitates from them, their pathological picture is described: signs of the naturalness or artificiality of the origin of the cuts are revealed, an analysis of the fluid oozing from them is studied, studied for color, transparency, consistency, impurities.
- The amount of fluid in the body cavity is measured and its properties are characterized. The condition of the serous membranes is examined and organ abnormalities with identified pathological foci of occurrence are described.
- If necessary, individual organs are measured in length and thickness with a ruler, and in some situations weighing is performed.
- In the case of the description of paired organs, a general characteristic is initially given, and then the changes in each of them are described.
- The general characteristic of focal changes and their morphological structure are necessarily displayed.At the same time, it is highly recommended not to use subjective assessments in the study, therefore, no official document of such a plan contains words of the type “normal”, “normal”, “in a state of dystrophy”, “hypertrophied” and so on. Also phrases like: “without visible deviations”, “without special damage” are not allowed.
Visual inspection
As for section A (external examination), the signs of cadaveric changes that were revealed during visual inspection of the corpse are reflected here. The special part describes:
- the appearance of the corpse;
- its location;
- physique of the deceased;
- weight;
- options;
- fatness;
- skin and its derivatives of subcutaneous tissue;
- visible mucous holes;
- the condition of the mammary glands (if the deceased is female);
- superficial lymph nodes;
- salivary glands;
- external genitalia;
- skeletal muscle;
- limbs.
Thus, during recording during an external examination of a corpse, a description of the cognitive signs of cadaveric changes in a person who died or died a natural death is described. A general examination of the body involves conducting and fixing the following procedures in a document:
- The study of the position of the body, its condition as a whole.
- Post-mortem changes are noted.
- Assessed cooling - complete, uniform, uneven, incomplete.
- Rigor mortis is examined - well-defined, weakly expressed or unexpressed.
- Cadaveric spots are identified, their location, shape, size, color.
- Posthumous blood coagulation is studied - the degree, consistency, color of the bundles, their separation from the walls of blood vessels, the state of the surface of the bundles.
- The degree of cadaveric decomposition is considered - autolysis (decay) has already arrived or not, a localized likely degree of severity.
- The body is examined for gas, discoloration, and odor.
- We study the pattern of tissue at the site of injury (in the event of violent death).

Internal inspection
Internal inspection (section B) provides for two documentation schemes in the protocol of the narrative:
- on anatomical systems and physiology;
- on the anatomical cavities of the body.
Such an inspection is deemed deeper, more detailed, large-scale. He very thoroughly and in detail considers in the smallest subtleties all the nuances with all the abnormal changes inside the body of the deceased and includes:
- analysis of the organs of the head and neck;
- examination of the chest, abdomen and pelvic cavity;
- examination of the skull, ridge and limbs.
The final part: the diagnosis
The final stage in recording the postmortem autopsy is considered to be the writing of the final part. The pathological diagnosis, the results of laboratory tests, as well as the conclusion about the causes of death (natural death) of a person are entered here.
The diagnosis is made in a certain order listing all examined and discovered during autopsy pathological terms. The specifics and essence of the reasons for the death that has occurred are important here. The diagnosis is made on the basis of the described changes that were discovered during the autopsy, so each item must correspond to and proceed from the descriptive part of the protocol. Post-mortem changes in the pathological diagnosis are not described because they were all reflected in the previous section of this document. This should not be just a list of changes, symptoms, syndromes detected during autopsy. All elements of the diagnosis should be presented in a logical sequence, taking into account the pathogenetic principle. It should be brief, specific, not allowing the omission of various manifestations of the pathological process.

Final part: conclusion
To establish the underlying disease, it is necessary to analyze the ailment and its accompanying processes, which is the basis of the medical conclusion. In contrast to the narrative, the organs should not be described here: the terms that have direct scientific and medical significance and reveal the clinical characteristics of the disease (violent death) of the deceased are specifically reflected here. For example, there may be definitions from terminology such as “liver necrosis”, “protein neurosis”, “catarrhal enteritis” and other pathologies identified in the organs.
The conclusion of the protocol (clinical and pathological epicrisis) is its most crucial part, which summarizes the results of the study. This is the paragraph of the final section of the autopsy report, which reflects the results of the examination for the cause of death, etiological and pathogenetic history due to established diseases and pathological changes that took place at the time of the laboratory examination. The conclusion is made on the basis of the diagnosis, anamnestic and genetic indicators.
Additional research
In cases where, based on the clinical signs and results of the postmortem autopsy, it is impossible to conclude the cause of a person’s death, that is, it is not possible to establish an accurate diagnosis, additional studies are being carried out. To do this, additional materials are taken for research and, according to the rules of documentation, a supporting document is filled out, the form of which determines the results of studies of histological, chemical, bacteriological bioassays. They are recorded in the protocol in the absence of missing results and specify the specifics of the studies that need to be done to clarify or confirm the pathological diagnosis.
